You know that feeling where you gotta go and you don’t know if you are going to make it to the toilet? Or on the other side of the road, it is day three and you still have not gotten that joyful release from your colon? How about abdominal cramping and gas that doubles you over in pain? And, we don’t really want to get into the nitty-gritty details of what does come out when things do move. When this is your world experience, you clearly know all is not right down below. But when you go to your doctor and tell him or her all about it, it is like you are talking to your hand – it looks like it should be useful, but it’s not. The usual advice is either to take Metamucil and drink more water or take Imodium. Sometimes they will throw in an antidepressant as obviously you are stressed. You dutifully follow their advice and guess what, nothing changes.
You know that feeling where you gotta go and you don’t know if you are going to make it to the toilet? Or on the other side of the road, it is day three and you still have not gotten that joyful release from your colon? How about abdominal cramping and gas that doubles you over in pain? And, we don’t really want to get into the nitty-gritty details of what does come out when things do move. When this is your world experience, you clearly know all is not right down below. But when you go to your doctor and tell him or her all about it, it is like you are talking to your hand – it looks like it should be useful, but it’s not. The usual advice is either to take Metamucil and drink more water or take Imodium. Sometimes they will throw in an antidepressant as obviously you are stressed. You dutifully follow their advice and guess what, nothing changes.
 This is daily life for over 60 million Americans. That is one in every five folks you run into. Learning to deal with this condition requires a major effort. I saw some of this effort when I went to the Colitis Foundation website to start my research for this article. For my purposes, I see colitis, Crohn’s, and IBS as variations of the same general patterns of disease, even though they each have their own special differentiating qualities. For instance, did you know that the effort has been made to create an app for your phone to identify the nearest bathroom to you wherever you are in case you have a sudden attack? That is really helpful for a lot of people.
This is daily life for over 60 million Americans. That is one in every five folks you run into. Learning to deal with this condition requires a major effort. I saw some of this effort when I went to the Colitis Foundation website to start my research for this article. For my purposes, I see colitis, Crohn’s, and IBS as variations of the same general patterns of disease, even though they each have their own special differentiating qualities. For instance, did you know that the effort has been made to create an app for your phone to identify the nearest bathroom to you wherever you are in case you have a sudden attack? That is really helpful for a lot of people.
 I almost decided not to tackle this topic after I spent an afternoon researching it. There are so many different ideas and so many different aspects to this disorder that it looks like an endless pit of chaos. Nobody really knows what the heck is going on. Different aspects are studied and identified, but the reality is that this is not a single disease. Every patient has their own personal set of causes and consequences. There is a genetic component sometimes. Stress definitely appears to be able to trigger flareups. Food is a big factor for many people, but not all. Hormone imbalances play into the mix. Parasites, viral infections, bacterial infections, and fungus sometimes trigger the problem, and other times are unrelated. There are definitely disturbances in the microbiome present, which may be a consequence or maybe a cause. Heavy metal toxicity, smoking, drinking, and drug use are known factors associated with the appearance of these symptoms. Pesticides, agricultural chemicals, smog/air pollution, food preservatives, coloring agents, plastics, and so on and so on all have been shown to contribute to colitis and its cousin conditions. We are dealing with seriously multi-variable causation confounded by individual patient-specific differences.
I almost decided not to tackle this topic after I spent an afternoon researching it. There are so many different ideas and so many different aspects to this disorder that it looks like an endless pit of chaos. Nobody really knows what the heck is going on. Different aspects are studied and identified, but the reality is that this is not a single disease. Every patient has their own personal set of causes and consequences. There is a genetic component sometimes. Stress definitely appears to be able to trigger flareups. Food is a big factor for many people, but not all. Hormone imbalances play into the mix. Parasites, viral infections, bacterial infections, and fungus sometimes trigger the problem, and other times are unrelated. There are definitely disturbances in the microbiome present, which may be a consequence or maybe a cause. Heavy metal toxicity, smoking, drinking, and drug use are known factors associated with the appearance of these symptoms. Pesticides, agricultural chemicals, smog/air pollution, food preservatives, coloring agents, plastics, and so on and so on all have been shown to contribute to colitis and its cousin conditions. We are dealing with seriously multi-variable causation confounded by individual patient-specific differences.
 Colitis reminds me very much of the profound work done by Dr. Bredesen in pinpointing 35 different causes for Alzheimer’s. In each dementia patient, any or any combination of the causes has to be addressed to relieve the condition. Each patient is unique and has to be evaluated for each and every possible cause and each cause has to be then eliminated to get resolution. This is what we are seeing with colitis – lots of potential and partial causes that combine together to create the final disease manifestation. Now you know why your average doctor looks blankly at you when you complain of gut issues. It is just too complex. Modern medicine is a name it, blame it, and tame it game. Give the complaint a name, give a predesignated single cause to blame it on, and prescribe a drug to tame that cause. Colitis does not yield to that game.
Colitis reminds me very much of the profound work done by Dr. Bredesen in pinpointing 35 different causes for Alzheimer’s. In each dementia patient, any or any combination of the causes has to be addressed to relieve the condition. Each patient is unique and has to be evaluated for each and every possible cause and each cause has to be then eliminated to get resolution. This is what we are seeing with colitis – lots of potential and partial causes that combine together to create the final disease manifestation. Now you know why your average doctor looks blankly at you when you complain of gut issues. It is just too complex. Modern medicine is a name it, blame it, and tame it game. Give the complaint a name, give a predesignated single cause to blame it on, and prescribe a drug to tame that cause. Colitis does not yield to that game.
 So what are we to do? If you were (or are) the patient with a life-altering condition, what would you do? Most colitis patients travel from one doctor to the next looking for answers. If you are fortunate enough to run into a functional medicine doctor and you have the resources and patience to look at all the possible causes and address them, you stand a good chance of conquering this condition. The correction may even be simple once you identify just what the triggering problems are in your case. But the journey to reach that point is usually a long one. This is why I hesitated to even write about this condition. I like to bring hope for feeling better through this newsletter, and I did not know what I could add to the conversation that was simple enough that my patients could try for themselves. I have a very much “do it yourself” attitude toward health. Doctors are good for emergency medicine. They are great at that. But health takes way more time and effort than they have office time for. Our health is up to us.
So what are we to do? If you were (or are) the patient with a life-altering condition, what would you do? Most colitis patients travel from one doctor to the next looking for answers. If you are fortunate enough to run into a functional medicine doctor and you have the resources and patience to look at all the possible causes and address them, you stand a good chance of conquering this condition. The correction may even be simple once you identify just what the triggering problems are in your case. But the journey to reach that point is usually a long one. This is why I hesitated to even write about this condition. I like to bring hope for feeling better through this newsletter, and I did not know what I could add to the conversation that was simple enough that my patients could try for themselves. I have a very much “do it yourself” attitude toward health. Doctors are good for emergency medicine. They are great at that. But health takes way more time and effort than they have office time for. Our health is up to us.
 My answer to my question is that there are some simple things colitis sufferers can try based on the physiology of what is going on that may provide relief for a good portion of them. Some percentage will need to do extensive lab testing and go down the long road to find a solution, but many will not need that much. So let’s look at some simple things to try. These conditions are all basically inflammation of the GI tract due to overreactions of the immune system in that area. Sometimes this is autoimmune in nature and other times auto-inflammatory – just a way of saying that different parts of the immune system have gotten upset. So what upsets the immune system in the gut?
My answer to my question is that there are some simple things colitis sufferers can try based on the physiology of what is going on that may provide relief for a good portion of them. Some percentage will need to do extensive lab testing and go down the long road to find a solution, but many will not need that much. So let’s look at some simple things to try. These conditions are all basically inflammation of the GI tract due to overreactions of the immune system in that area. Sometimes this is autoimmune in nature and other times auto-inflammatory – just a way of saying that different parts of the immune system have gotten upset. So what upsets the immune system in the gut?
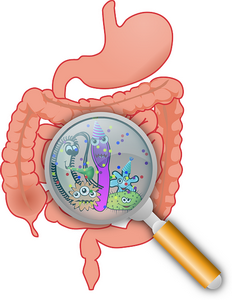 The immune system in the gut is there to stop bad guys and bad stuff from getting into the bloodstream. When the immune system gets angry, it is because it thinks bad guys/stuff are going where it does not belong. Usually, this is because that is exactly what is happening. What turns this unfortunate occurrence into a disease is when this keeps happening over and over. When you get food poisoning you basically get an immediate short-term irritable bowel syndrome. You throw up, you have diarrhea, you get rid of the poison and bad bacteria, and you recover. But when you chronically inflame the gut by eating bad foods, being over-stressed, breathing in poisons from your toxic environment, feeding bad guy bacteria in your gut, not getting restorative sleep, and having poor digestion, eventually you end up with a named gut disease. Some of you will have a greater genetic susceptibility to these types of problems. Others will have jobs that set you up for this. Let’s start with the “easy stuff” first.
The immune system in the gut is there to stop bad guys and bad stuff from getting into the bloodstream. When the immune system gets angry, it is because it thinks bad guys/stuff are going where it does not belong. Usually, this is because that is exactly what is happening. What turns this unfortunate occurrence into a disease is when this keeps happening over and over. When you get food poisoning you basically get an immediate short-term irritable bowel syndrome. You throw up, you have diarrhea, you get rid of the poison and bad bacteria, and you recover. But when you chronically inflame the gut by eating bad foods, being over-stressed, breathing in poisons from your toxic environment, feeding bad guy bacteria in your gut, not getting restorative sleep, and having poor digestion, eventually you end up with a named gut disease. Some of you will have a greater genetic susceptibility to these types of problems. Others will have jobs that set you up for this. Let’s start with the “easy stuff” first.
 The simplest type of digestive inflammation comes from the after effects of eating something that your system believed was either contaminated with a bad bacteria or poison or that you are allergic to. When this happens your gut opens up all its control valves (cardiac, pyloric, ileocecal, and internal rectal) and tries to dump everything out to protect you. Sometimes when this happens one or more valves get stuck open which then compromises the function of the gut. I adjust these issues every day in the office and usually get resolution of the gut issues at least half the time within a couple days.
The simplest type of digestive inflammation comes from the after effects of eating something that your system believed was either contaminated with a bad bacteria or poison or that you are allergic to. When this happens your gut opens up all its control valves (cardiac, pyloric, ileocecal, and internal rectal) and tries to dump everything out to protect you. Sometimes when this happens one or more valves get stuck open which then compromises the function of the gut. I adjust these issues every day in the office and usually get resolution of the gut issues at least half the time within a couple days.
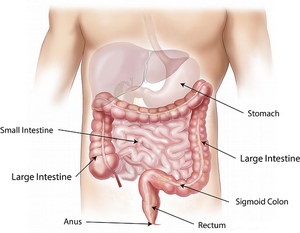 If this type of problem has been in place for too long you may develop what is called SIBO – Small Intestinal Bacterial Overload. This happens when the ileocecal valve between the last part of the small intestine and the colon gets stuck open and bacteria from the colon backs up into the small intestine. Obviously the valve needs to be adjusted to reset it, but you then need to follow what is called a FODMAP diet for a month or two to get rid of the excess bacteria that has set up shop in the small intestine. Here is a copy of that diet. You want low FODMAP foods to starve out the excess bacteria.
If this type of problem has been in place for too long you may develop what is called SIBO – Small Intestinal Bacterial Overload. This happens when the ileocecal valve between the last part of the small intestine and the colon gets stuck open and bacteria from the colon backs up into the small intestine. Obviously the valve needs to be adjusted to reset it, but you then need to follow what is called a FODMAP diet for a month or two to get rid of the excess bacteria that has set up shop in the small intestine. Here is a copy of that diet. You want low FODMAP foods to starve out the excess bacteria.
Digestion: crappy digestion equals crappy gut health. Let’s start at the top:
 Do you chew your food enough to get fully salivary enzyme action?
Do you chew your food enough to get fully salivary enzyme action?
Do you have enough stomach acid to break down your food?
Do you have enough pancreatic enzymes to digest your food?
Do you have good bile flow to digest your fats?
These can be checked by taking various supplements to compensate.
Are you relaxed when you eat so the gut nerves can work?
Are you eating lectins or anti-nutrients from plants that stop digestion and promote inflammation?
Are you eating evil gut bug foods like sugar and toxic vegetable oils?
Are you eating gut poisons like gluten, alcohol, glyphosate, food chemicals, etc.?
 These types of problems generally create what is called Leaky Gut, which allows these various poisons to cross over the gut wall and into the blood stream, triggering the immune system into hyper activity. My first level of therapy is to avoid the biggest offenders in the diet for three months and see if that is enough to resolve the problem. For this I use a diet protocol I created which you can find here.
These types of problems generally create what is called Leaky Gut, which allows these various poisons to cross over the gut wall and into the blood stream, triggering the immune system into hyper activity. My first level of therapy is to avoid the biggest offenders in the diet for three months and see if that is enough to resolve the problem. For this I use a diet protocol I created which you can find here.
If this is not clean enough to create resolution we will step up to fasting, or if the first four digestive concerns are addressed, a carnivore diet for a month.
 You can self-assess your sleep quality. You absolutely need 71/2 to 8 hours of good quality sleep every night – no excuses. Stress is everywhere, but the choice to nurture yourself and give yourself time to relax and rejuvenate requires a significant commitment to your health over your other stress-inducing concerns. I tell myself, that if I don’t take care of myself first, then I don’t have anything with which to take care of all the other concerns I have. My health comes first. A couple years ago I wrote an article about a simple 2 minute way to release stress with a simple vagus nerve reset – check it out here.
You can self-assess your sleep quality. You absolutely need 71/2 to 8 hours of good quality sleep every night – no excuses. Stress is everywhere, but the choice to nurture yourself and give yourself time to relax and rejuvenate requires a significant commitment to your health over your other stress-inducing concerns. I tell myself, that if I don’t take care of myself first, then I don’t have anything with which to take care of all the other concerns I have. My health comes first. A couple years ago I wrote an article about a simple 2 minute way to release stress with a simple vagus nerve reset – check it out here.
To check for infections, parasites, toxic burdens, hormonal imbalances, and the like will probably require extensive lab tests. So those possible causes I check after I eliminate the stuff from the self-tests. I estimate the self-testing and corrections will resolve maybe 60% of the Colitis/Crohns/IBS cases. So that is my contribution to the gut health conversation.
Good hunting,
David