
Have you ever wondered just what it is I really do? Yes, I am a Doctor of Chiropractic, but that doesn’t really say anything about what I actually am doing when you come in for a visit. You know from experience that your pain decreases and your function improves, and that is really the point. But sometimes curiosity arises around what did I change to make that happen. Why would you care? Knowing what is “going on behind the curtain” can help you support the changes being made, or at least understand why not to do certain things that will mess up ‘the adjustment’.

For over a hundred years Chiropractors have been telling the story that what Chiropractors do is “remove nerve interference by removing vertebral subluxations through spinal manipulation.” They then go on to explain how your spinal bones can get ‘out of place’ and put pressure on the nerves causing dysfunction, much like stepping on a hose stopping the flow of water. The bone pressing on the nerve analogy has been passed around so long that most people have come to believe that the analogy is the same as the truth. Analogies are not the truth, they merely show similarity in one respect. In the old days, there was much discussion as to just what a subluxation really was. The anatomists of the day knew that bones did not really get ‘out of place’ ordinarily, as bones are all tied together by really tough ligaments. If the joint is damaged sufficiently to tear those ligaments, you get luxations or dislocations, such as what happens in some shoulder or knee injuries.
Early anatomical studies on living creatures demonstrated the decreased firing of nerve impulses down a nerve when very small pressures were applied to the nerve within the first centimeter of the spine. Likewise, these decreased nerve firings were demonstrated to produce muscle weakness or spasticity, disrupt organ function, and scramble hormonal activity. These issues were the same issues that early Chiropractors found that their spinal adjustments corrected. The obvious mental leap is that the adjustment must be fixing similar pressure on nerve roots. Evidence exists that this may actually be true some percentage of the time. The trouble has always been the part about the bone being ‘out of place’ causing the pressure on the nerves. It is a simple easy to understand model, but it does not stand up to the physical reality of how joints are constructed. Nothing in life is that simple, and that applies to the old stack of bones being “out of place’ story as well. The analogy helps to explain what is going on to the average patient of the last century, but modern patients are much more proactive and want to participate in their own care. So it is time to update the model to facilitate patient participation. Let’s do that.
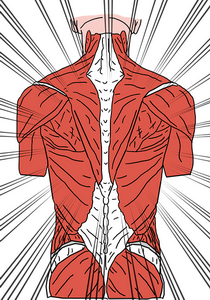
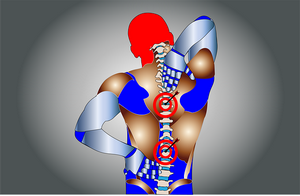
Obviously, bones move. If they didn’t we would be frozen in place. Bones all have a normal range of movement limited by stabilizing ligaments, adjacent bones, and muscle/tendon connections. In the spine, you have seven layers of muscles, with each layer pulling in a different direction on the spinal vertebra. This produces eight directions of movement in four planes – up/down, right/left rotation, right/left lateral motion, and left side down/right side down motion. A few places in the spine can also move forward and backward. That is a lot of muscle action that is incredibly complex in how it has to be coordinated to allow you to move your spine around. Compare this to your elbow, which has only one plane of movement – open and closed. The triceps muscle opens the elbow joint and the biceps muscle closes the elbow joint – simple. The spine is crazy complex, and like anything crazy complex, the more complex it is the easier it is for something to go wrong. Too many things have to work perfectly all simultaneously for the simplest movement. Guess what, glitches happen. When they do, tiny muscles spasm causing asymmetric compression of joints, which produces pain, swelling, inflammation, and – here it comes – nerve compression due to the swelling.
This is part of the real story behind the old school “pressure on the nerves from the bones being out of place” line. You can get real bone pressure on nerves from such things as disc degeneration between the vertebra, or spinal stenosis where the inside of the vertebra grows to put pressure on the spinal cord, or of course traumatic injury.
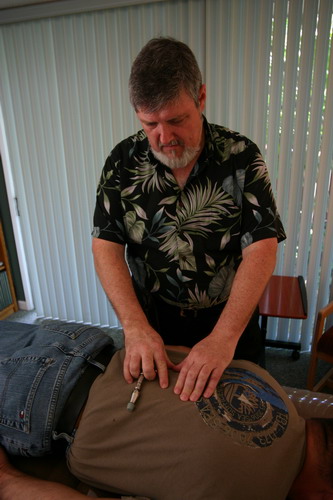
So what am I doing when you come in to see me? Well, you walk in and draw a picture of where your pain is. I ask you a few questions to see how this is affecting your functioning. I feel the area for the swelling and the spasms on a minute level. And I use muscle testing to challenge the area to see what directions of challenge trigger the inflammation reaction in the sensory nerves in that area. This is just what I outlined above as the consequence of the joint “glitch” causing the issue – spasm, pain, swelling, and inflammation. From this exam, I determine just which tiny muscles are not functioning correctly, and then use the high-speed low impact Activator adjustments to correct the functioning of the muscles. If this is a very recent “glitch” then often the relief is instantaneous as muscle balance is restored and normal function returns. If there has been too much time or the spasm has produced a great deal of joint pressure, there may be joint swelling and inflammation that will have to come down to produce the desired result. When this is the case, I recommend the use of heat followed by cold to flush out the inflammation and reduce the swelling.Now for the geek level of understanding – what does the adjustment do? Here we have to get into a bit of neurology to unpack this concept. Every muscle and every joint has specialized nerve endings in them that continuously feedback to the brain every change in

tension. The brain tries to keep track of just how tight every tendon is, how long or short every muscle is, and how much stress is being applied to every ligament. From this information, your brain keeps a moment to moment map of where all your parts are and what they are doing. This is where the patient participation part of health maintenance comes into play. Nerves are like paths in the forest. Paths that are used only a few times a day are very faint and tiny. Paths that are used hundreds of times each day are strong, bold, and clear. As your brain tries to keep an updated map of where everything is, it depends on good strong signals coming from all the joints and muscles. So if you are not moving lots and lots, your paths are like the faint and tiny forest paths. Those signals do not form a good strong map for the brain, and without a good strong map, your brain does not know how to adapt to and compensate for changes that affect your body. When you get up from sitting, your brain has to compensate for the front muscles in your lap having contracted while you were sitting. As you get up, those contracted muscles will yank the

low back forward, possibly jamming your low back joints. With a good strong map, your brain will tell the low back stabilizer muscles to tighten up to compensate for the contracted lap muscles, thus preventing injury. This is one tiny example of the thousands of compensations and adaptations your brain has to do every day to keep your joints moving smoothly.


The nerves that form this map for coordination and muscle balance are called proprioceptive nerves. Like muscles, they grow and shrink with use. They need a lot of use to stay strong and functional. When I make an adjustment, what I am actually doing is changing the feedback these nerves are making to the brain. I can turn up or down the signals they are sending to the brain. A single click of the Activator tool has been measured to increase proprioceptive firing over a hundredfold for a few milliseconds. This rewires the brain map by giving it a big jolt of information. The brain then makes the actual adjustment to the muscles to bring balance to the joint. Essentially I am adjusting your brain map of where you are in space. This all has fancy neurological names and complex processes we would not find useful as patients receiving adjustments. The important part is how vital it is to keep moving. Movement is what stimulates the body to build more and better nerve paths. You want to keep those pathways clear and strong. Also important is keeping inflammation down with the use of the heat followed by cold. Muscles like heat and the joints like cold, so if you find that just heat or cold works better alone, that tells us where the main problem is. While joints are swollen and inflamed, the nerve signals are easily scrambled and the joint is unstable. This means it is very easily re-injured or fired up. So we have to find the sweet spot of keeping the area moving without straining the joint and further injuring it. Complete rest is rarely indicated unless there is massive ligament tearing in the area. Even then we need micro-movements to flush out the swelling so new blood and nutrients can get to the area to promote healing.

So that is the story of what I am doing when you come into the office for an adjustment. I am literally reprogramming the faulty signals to your brain so that your brain can bring the joints back into functional balance. Soft tissues follow the same paradigm when I work with them. Everything I do is about clarifying the communication between your brain and your body. Glitches happen for lots of reasons. How to fix those glitches is way too complex for me to figure out, so I clear up the communication between your brain and the glitch and let your brain do the hard work to fix it. Your body knows how to heal itself. That is the real magic.
Take care,
David
