I’ve been a doctor for over four decades, and I can tell you something has definitely changed in my practice sin ce 2020. The number of patients coming in complaining of dizziness, vertigo, and balance problems has skyrocketed. Before 2020 I would see 2 or 3 cases of vertigo a year. Now it is common to see 2 or 3 a day! If you’re dealing with this yourself, you’re not imagining it—and you’re definitely not alone. Let me explain what we’re seeing, why COVID seems to be behind much of it, and most importantly, what you can do about it at home. ce 2020. The number of patients coming in complaining of dizziness, vertigo, and balance problems has skyrocketed. Before 2020 I would see 2 or 3 cases of vertigo a year. Now it is common to see 2 or 3 a day! If you’re dealing with this yourself, you’re not imagining it—and you’re definitely not alone. Let me explain what we’re seeing, why COVID seems to be behind much of it, and most importantly, what you can do about it at home.
The Vertigo Epidemic Nobody’s Talking About
Walk into any primary care office these days, and “dizziness” is one of the top complaints. Some patients had COVID
 and never quite recovered. Others had what seemed like a mild case months ago but now can’t shake this spinning, off-balance feeling. And interestingly, some people never knew they had COVID at all but started having vertigo around the same time they got their second or third booster shot of spike protein to train their immune system to fight COVID. The statistics back this up. Studies show that anywhere from 15-30% of people with Long COVID report dizziness or vertigo as a persistent symptom. That’s millions of people worldwide dealing with a room that won’t stop spinning or a constant feeling of being on a boat. and never quite recovered. Others had what seemed like a mild case months ago but now can’t shake this spinning, off-balance feeling. And interestingly, some people never knew they had COVID at all but started having vertigo around the same time they got their second or third booster shot of spike protein to train their immune system to fight COVID. The statistics back this up. Studies show that anywhere from 15-30% of people with Long COVID report dizziness or vertigo as a persistent symptom. That’s millions of people worldwide dealing with a room that won’t stop spinning or a constant feeling of being on a boat.
How COVID Attacks Your Balance System
Here’s the thing about vertigo: it’s not one problem —it’s a symptom that can come from several different places. And unfortunately, COVID seems to have a knack for hitting multiple parts of your balance system at once. —it’s a symptom that can come from several different places. And unfortunately, COVID seems to have a knack for hitting multiple parts of your balance system at once.
Your Inner Ear
COVID can directly infect the delicate structures of your inner ear. The virus uses ACE2 receptors to get into cells, and your inner ear is loaded with these receptors. When the virus causes inflammation there, it can damage the tiny hair cells that detect movement and position, or it can affect the fluid balance in the semicircular canals—the organs responsible for sensing rotation and movement.
Some patients develop what we call vestibular neuritis, where the nerve connecting your inner ear to your brain gets inflamed. Others develop something similar to Meniere’s disease, with fluctuating symptoms, pressure in the ear, and sometimes ringing (tinnitus).
Your Nervous System
But here’s where it gets really challenging—and for many of you, this might be the key issue. COVID doesn’t just attack your inner ear; it messes with your autonomic nervous system. This is the part of your nervous system that runs in the background, automatically controlling things like heart rate, blood pressure, and blood flow.
When your autonomic nervous system goes haywire (a condition called dysautonomia), your blood pressure can drop when you stand up or change positions. Less blood reaches your brain and inner ear, and boom—vertigo. Your heart might race trying to compensate, you feel lightheaded, the room spins, and you might feel like you’re going to pass out. This is especially common in people who develop POTS (Postural Orthostatic Tachycardia Syndrome) after COVID. POTS is now one of the most recognized forms of Long COVID, and vertigo is one of its hallmark symptoms. My newsletter last week was all about this concern.
Your Brain
COVID can also affect the parts of your brain that pr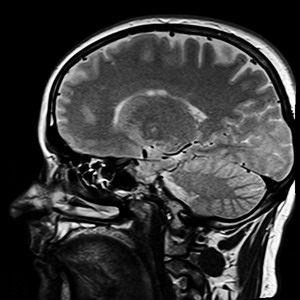 ocess balance information—particularly the brainstem and cerebellum. Even without obvious neurological damage, the inflammation COVID causes throughout your body can affect how these areas function. Some people describe it as persistent brain fog combined with a sensation that the ground is moving beneath them. ocess balance information—particularly the brainstem and cerebellum. Even without obvious neurological damage, the inflammation COVID causes throughout your body can affect how these areas function. Some people describe it as persistent brain fog combined with a sensation that the ground is moving beneath them.
What Type of Vertigo Do You Have?
This matters because the treatment is different depending on the cause. Let me help you figure out which type you might be dealing with.
Inner Ear Vertigo (BPPV, Vestibular Neuritis)
This type typically:
Causes intense spinning when you move your head 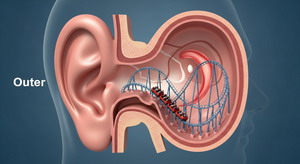 in certain positions. in certain positions.
Lasts seconds to minutes with position changes.
Might come with nausea that can be severe.
Often improves when you keep your head still.
May include ear fullness, hearing changes, or tinnitus.
Autonomic Vertigo (POTS, Dysautonomia)
This type typically:
Gets worse when you stand up or have been standing.
Improves significantly when you lie down.
Comes with a racing heart, especially when upright.
Is accompanied by fatigue, brain fog, or feeling flushed.
Might worsen in hot environments or after eating.
Often feels more like constant imbalance than spinning.
Central/Neurological Vertigo
This type typically:
Feels like persistent unsteadiness or “floating”.
Doesn’t change much with position.
May come with other neurological symptoms.
Can include visual disturbances or difficulty focusing.
Many COVID patients have a combination of these, which is why it can be so confusing and hard to treat.
What You Can Do at Home
The good news is that there are effective strategies you can start right now, regardless of which type you’re dealing with.
For Autonomic-Related Vertigo
Increase Your Salt and Water Intake
Move Slowly and Deliberately
Try Compression Garments
Keep Cool
This was discussed in detail last week. Here is a link to that article.
For Inner Ear Vertigo
The Epley Maneuver
If your vertigo is triggered by specific head positions  (like rolling over in bed or looking up), you might have BPPV—benign paroxysmal positional vertigo. This is caused by tiny crystals in your inner ear getting into the wrong place. The Epley maneuver is a series of head positions that can move these crystals back where they belong. Epley is the most common, but other maneuvers may be better for you. Others include the Semont maneuver, Brandt-Daroff exercises, Barbeque roll, Gufoni maneuver, and the Half-Somersault (Foster). You can find videos online that walk you through them, or better yet, see a physical therapist who specializes in vestibular rehabilitation. Many people get complete relief after just one or two treatments. (like rolling over in bed or looking up), you might have BPPV—benign paroxysmal positional vertigo. This is caused by tiny crystals in your inner ear getting into the wrong place. The Epley maneuver is a series of head positions that can move these crystals back where they belong. Epley is the most common, but other maneuvers may be better for you. Others include the Semont maneuver, Brandt-Daroff exercises, Barbeque roll, Gufoni maneuver, and the Half-Somersault (Foster). You can find videos online that walk you through them, or better yet, see a physical therapist who specializes in vestibular rehabilitation. Many people get complete relief after just one or two treatments.
Vestibular Rehabilitation Exercises
Even if you don’t have classic BPPV, vestibular exercises can help your brain compensate for inner ear dysfunction. Simple exercises like:
Focusing on a target while turning your head side to side.
Walking while turning your head.
Standing on one foot (near a wall for safety).
Tracking a moving object with your eyes.
These retrain your brain to process balance information better. Start slowly and expect to feel a bit worse initially—that’s actually a sign the exercises are working.
For Everyone
Get your head and neck adjusted
I am able to open up the blood flow to your brainste m to improve vestibular function on the brain level. I also check your eye muscle attachments for visual tracking errors caused by this issue. The balance of the neck muscles is also a key element of body balance so we need that working well also. m to improve vestibular function on the brain level. I also check your eye muscle attachments for visual tracking errors caused by this issue. The balance of the neck muscles is also a key element of body balance so we need that working well also.
Optimize Your Sleep
Your brain does a lot of healing and recalibrating during sleep. Aim for 8-9 hours in a cool, dark room. Elevate the head of your bed slightly (4-6 inches)—this can help with morning vertigo.
Stay Hydrated Throughout the Day
Not just water—you need electrolytes too. Coconut water, electrolyte drinks, or even just adding a pinch of salt to your water helps maintain the fluid balance in your inner ear.
Avoid Triggers
Common vertigo triggers post-COVID include:
Alcohol (even small amounts)
Caffeine (can worsen POTS symptoms)
High-sodium processed foods that cause blood sugar swings
Rapid head movements
Busy visual environments (crowds, scrolling on phones)
Stress and poor sleep
Consider Supplements
Some patients find benefit from:
Magnesium (helps with muscle tension and sleep)
Vitamin B12 (supports nerve function)
Ginger (natural anti-nausea properties)
Coenzyme Q10 (supports mitochondrial function)
When to See a Doctor
Most post-COVID vertigo improves with time and  these home strategies, but you should see a medical doctor if: these home strategies, but you should see a medical doctor if:
You have sudden severe vertigo with hearing loss (this is an emergency).
Your vertigo comes with severe headache, double vision, slurred speech, or weakness.
You’re fainting or nearly fainting regularly.
Your symptoms are getting progressively worse.
You’re not seeing improvement after 4-6 weeks of trying these strategies.
Your doctor can do testing to determine the exact cause and may prescribe medications like meclizine for nausea, beta-blockers for POTS symptoms, or refer you to a vestibular specialist.
The Bottom Line
If you’re dealing with vertigo after COVID, please kn ow that you’re not alone and you’re not crazy. This is a real, physical problem affecting millions of people. The connection between COVID and vertigo is becoming clearer every day, and while it’s frustrating, it’s usually treatable. ow that you’re not alone and you’re not crazy. This is a real, physical problem affecting millions of people. The connection between COVID and vertigo is becoming clearer every day, and while it’s frustrating, it’s usually treatable.
Start with the basics: more salt, more water, slower movements, and vestibular exercises. The literature says you should see meaningful improvement within 2-3 months of consistently applying these strategies. Your balance system got knocked off-kilter by COVID, but it can recalibrate. It just needs time, support, and the right approach. Be patient with yourself, track what helps, and don’t hesitate to seek professional help if you need it.
We took a little break from all the work lately, and actually went out to a movie and lunch. It seems we hardly get out o f the house these days, and we have not been to a movie in almost a year. Here we are at our favorite Vietnamese restaurant out in Rancho Cordova – Pho Fresh. f the house these days, and we have not been to a movie in almost a year. Here we are at our favorite Vietnamese restaurant out in Rancho Cordova – Pho Fresh.
Best exercise for knee osteoarthritis

So is it cardio, weights, stretching, balance, mind-body? After comparing 200 studies the winner is aerobic training like walking, bicycling, or swimming. They were twice as effective as the next runner up, strength training.
More
___________________________
“Principle of forgiveness. Anything we are in resistance to we are stuck with. Letting go of resentment allows us to move on and grow.“
~David DeLapp
_____________________________________
Singing for breathlessness
COPD and interstitial lung disease make simple breathin g a constant challenge. A new study found that group singing for 90 minutes once a week significantly improved patients ability to breathe. g a constant challenge. A new study found that group singing for 90 minutes once a week significantly improved patients ability to breathe.
More
____________________________
“Principle of gratitude. Appreciating what is in your life builds a perception of value and open the doors to receiving the gifts and learning it offers.“
~David DeLapp
________________________________________
Proscar and Propecia markedly increase depression and suicide risk
Hair loss drugs block an enzyme that converts testost erone into a form that shrinks hair follicles. Unfortunately that same enzyme is responsible for the formation of a hormone that regulates mood. erone into a form that shrinks hair follicles. Unfortunately that same enzyme is responsible for the formation of a hormone that regulates mood.
More
________________________
“Natural Life is always fair even though it may not be the way you like. You always get/have just what you deserve, because it is what you have created. Your life is your reflection.“
~David DeLapp
|
|
|
|
|

