If you’re dealing with Long COVID, you’ve probabl y noticed some weird stuff happening with your body. Your heart races when you stand up. You get winded doing things that used to be easy. You feel dizzy, exhausted, or just “off” in ways that are hard to explain. A lot of this could be autonomic dysfunction—basically, your nervous system isn’t regulating things like heart rate and blood pressure the way it should.
y noticed some weird stuff happening with your body. Your heart races when you stand up. You get winded doing things that used to be easy. You feel dizzy, exhausted, or just “off” in ways that are hard to explain. A lot of this could be autonomic dysfunction—basically, your nervous system isn’t regulating things like heart rate and blood pressure the way it should.
Here’s the good news: you can do some simple tests at home to track what’s going on. All you need is a pulse oximeter (that little clip thing that goes on your finger) and a timer. Let’s walk through it.
The Breath-Hold Test: Simpler Than It Sounds
The breath-hold test is exactly what it sounds like— you hold your breath and time how long you can last. It might seem too simple to be useful, but it actually tells you a lot about how your cardiovascular, respiratory, and nervous systems are working together.
you hold your breath and time how long you can last. It might seem too simple to be useful, but it actually tells you a lot about how your cardiovascular, respiratory, and nervous systems are working together.
Here’s how to do it:
1.Sit comfortably and rest for about 5 minutes. Jus t breathe normally and relax.
t breathe normally and relax.
2.Take a normal breath in, then breathe in a bit more until your lungs feel comfortably full—not bursting, just full.
3.Hold your breath and pinch your nose (no cheating!). Start your timer.
4.Hold until you absolutely have to breathe. Don’t try to be a hero—stop when your body is screaming at you that it needs air.
5.Record your time and note how you felt. Was it just uncomfortable, or did you feel panicky? Did your heart pound?
6.Wait 3-5 minutes and try it two more times. You’ll get slightly different numbers each time—that’s normal.
What This Test Actually Shows
When you hold your breath, carbon dioxide builds up in your blood. Your body has sensors (chemoreceptors) that detect this and tell your brain “Hey, we need to breathe NOW.” In people with Long COVID, these sensors often become oversensitive. It’s like they’re set on a hair trigger.
You might also notice:
Your heart racing during the breath-hold
Feeling panicky or anxious
An overwhelming sensation of needing air way sooner than you expected
Feeling shaky or weird afterward
These reactions suggest your autonomic nervous system is in overdrive—specifically, your sympathetic nervous system (the “fight or flight” mode) is too active, while your parasympathetic system (the “rest and digest” mode) isn’t doing its job to calm things down.
Adding the Pulse Oximeter: More Information
Now let’s make this test even more useful by adding a pulse oximeter. These little devices cost $20-40 and clip onto your finger. They show two numbers: your oxygen saturation (SpO2) and your heart rate.
Enhanced breath-hold test with pulse oximeter:
1.Clip the pulse oximeter on your finger before you start.
2.Note your resting heart rate and oxygen level (should be 95-100% for oxygen, and heart rate varies but maybe 60-90 beats per minute at rest).
3.Do the breath-hold test while watching the numbers.
4.Keep the oximeter on for 2-3 minutes after you start breathing again to see how things recover.
What to watch for:
Your oxygen saturation will usually stay pretty sta ble during a breath-hold (maybe dropping to 92-95% at most). If it drops lower, that could suggest lung issues. But the really interesting number is your heart rate.
ble during a breath-hold (maybe dropping to 92-95% at most). If it drops lower, that could suggest lung issues. But the really interesting number is your heart rate.
In people with autonomic dysfunction, you’ll often see:
Heart rate jumping up 20-30 beats or more during the breath-hold
Heart rate staying elevated for a while after you start breathing
Feeling your heart pounding even though you’re sitting still
A disconnect between how you feel and what the numbers show
The Standing Test: Catching POTS
While we’re at it, let’s do one more simple test that can spot POTS (Postural Orthostatic Tachycardia Syndrome), one of the most common forms of autonomic dysfunction in Long COVID.
How to do it:
1.Lie down for 5 minutes. Relax completely.
2.With your pulse oximeter on, note your heart rate while lying down.
3.Stand up and immediately check your heart rate. Keep standing and check it again at 2, 5, and 10 minutes.
4.Write down all these numbers.
What it means:
If your heart rate increases by 30 beats per minute o r more within 10 minutes of standing (or 40+ if you’re a teenager), that meets the criteria for POTS. For example, if you’re at 70 lying down and hit 100+ when standing, that’s significant.
r more within 10 minutes of standing (or 40+ if you’re a teenager), that meets the criteria for POTS. For example, if you’re at 70 lying down and hit 100+ when standing, that’s significant.
You might also notice:
Feeling dizzy or lightheaded
Vision getting blurry or spotty
Heart pounding in your chest
Feeling like you might faint
Brain fog getting worse when upright
What To Do If Your Tests Look Abnormal

Okay, so you’ve done these tests and things don’t look great. Your breath-hold time is short, your heart is racing, and standing up makes you feel terrible. Now what?
First, don’t panic. Autonomic dysfunction is real and it’s miserable, but there are things you can do at home that really help. Here are the most effective strategies:
1. Salt and Water (Seriously, This Helps)
This sounds too simple to work, but for many people, it’s life-changing.
Increase your salt intake to 6-10 grams per day. That’s about 2-3 teaspoons. You can use salt tablets (easier to track), add salt to everything you eat, drink pickle juice, eat salty snacks, or have bouillon cubes in hot water. When increasing salt intake, it is also important to increase your potassium intake just as much. My Balanced Salt has this correct ratio.
Drink 2-3 liters of water daily. Not all at once—spread it throughout the day.
Why does this work? Salt and water increase your blood volume, which helps prevent blood from pooling in your legs when you stand up. More blood volume means better blood flow to your brain and less compensatory racing of your heart.
Important: Check with your doctor first if you have high blood pressure, heart failure, or kidney problems.
2. Compression Garment s
s
Get yourself some waist-high compression stockings (20-30 mmHg) or an abdominal binder. Yes, they’re uncomfortable and annoying to put on, but they work.
Put them on before you get out of bed in the morning (while you’re still lying down). They prevent blood from pooling in your legs and abdomen, which reduces that awful feeling when you stand up.
3. Change How You Move
Never jump straight out of bed. Instead:
Roll to your side 
Sit up slowly and dangle your legs
Pump your ankles up and down 10-20 times
Wait a minute or two
Stand slowly
Wait another 30 seconds before walking
When standing, don’t stand still (that’s actually the worst position). Instead:
Rock back and forth
Shift your weight from foot to foot
Do calf raises
Cross your legs and squeeze your thighs
Lean against something
Better yet, sit on a tall stool instead
4. Exercise Lying Down
This sounds weird, but it’s crucial. When you have a utonomic dysfunction, upright exercise makes things worse. Start with exercise that keeps you horizontal:
utonomic dysfunction, upright exercise makes things worse. Start with exercise that keeps you horizontal:
Recumbent bike
Rowing machine (if you can recline)
Swimming (floating horizontally)
Floor exercises (leg lifts, bridges, arm movements)
Start with just 5-10 minutes and slowly build up. Keep your heart rate low—you’re not trying to train for a marathon, you’re retraining your nervous system.
If you currently crash with any activity then be sure you can do 30-45 minutes of horizontal exercise without crashing before you even think about upright activities like walking or regular biking.
5. Breathing Exercises
Remember how your nervous system is stuck in “fig ht or flight” mode? Breathing exercises can help flip it back to “rest and digest.”
ht or flight” mode? Breathing exercises can help flip it back to “rest and digest.”
Simple diaphragmatic breathing:
Lie down or sit comfortably
Put one hand on your chest and one on your belly
Breathe in through your nose, making your belly rise (chest shouldn’t move much)
Breathe out slowly through your mouth
Make your exhale twice as long as your inhale
Do this for 5-10 minutes, 3-4 times a day
This activates your vagus nerve, which is like the master switch for calming your nervous system down.
6. Keep Your Cool
Many people with autonomic dysfunction can’t handle heat well. Hot showers, hot weather, and hot rooms all make  symptoms worse.
symptoms worse.
Take lukewarm showers (use a shower chair)
Keep your house cool
Use fans liberally
Wear light, breathable clothing
Exercise in the coolest part of the day
7. Eat Small, Frequent Meals
Big meals divert blood to your digestive system, which can make you feel dizzy and exhausted (postprandial hypotension). Instead, eat 5-6 small meals throughout the day. Avoid high-sugar foods that cause blood sugar swings—those make autonomic symptoms worse.
Tracking Your Progress
Do these tests weekly and write down your results. You’re looking for trends:
Is your breath-hold time increasing?
Is your heart rate less reactive?
Can you stand longer without symptoms?
Are you tolerating more activity?
Progress is usually slow—think months, not weeks. You’ll have good days and bad days. That’s normal. The key is the overall trend over time.
When to See a Doctor
These home tests and strategies can help a lot, but they’r e not a substitute for medical care. See a doctor if:
e not a substitute for medical care. See a doctor if:
You’re fainting or nearly fainting regularly
You have chest pain or concerning palpitations
Your symptoms are getting worse despite trying these strategies
You can’t maintain basic self-care
Your breath-hold time is under 10 seconds
Ask about seeing a cardiologist or an autonomic specialist. There are medications that can help (like beta-blockers, ivabradine, or midodrine), but lifestyle modifications should be tried first.
The Bottom Line
Long COVID autonomic dysfunction is real, measura ble, and manageable. You’re not imagining it, you’re not crazy, and you’re not alone. These simple tests—breath-holding with a pulse oximeter and the standing test—can give you objective data about what’s happening in your body.
ble, and manageable. You’re not imagining it, you’re not crazy, and you’re not alone. These simple tests—breath-holding with a pulse oximeter and the standing test—can give you objective data about what’s happening in your body.
More importantly, the basic strategies of salt, water, compression, horizontal exercise, breathing exercises, and smart pacing can make a huge difference. Most people see meaningful improvement within 3-6 months of consistently doing these things.
Your nervous system got knocked out of whack by COVID, but it can recover. It just needs time, support, and the right approach. Start with these simple tests to understand what’s going on, then give your body what it needs to heal. You’ve got this.
Take care,
Ellen
Ellen has had a wide variety of life experiences. Back about 40 years ago, between husbands 4 and 5, she had a career as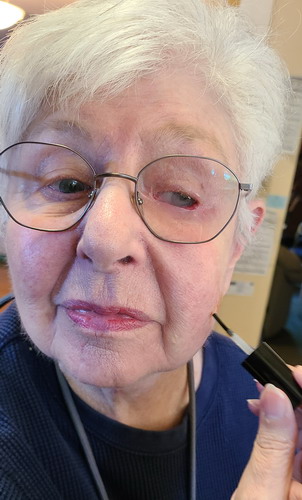 an esthetician. That experience has stuck with her and to this day she is always experimenting with different facial care products. Recently someone told her that my Fungi Stop product would take away brown spots on the skin. Naturally she wanted to experiment with it to see if it actually works. Here she is putting some on a small spot on her left cheek. We shall see if it takes the spot away. So far the last couple of days it seems to be acting like a dermal peeling agent. The area gets dry and a layer of skin peels off.
an esthetician. That experience has stuck with her and to this day she is always experimenting with different facial care products. Recently someone told her that my Fungi Stop product would take away brown spots on the skin. Naturally she wanted to experiment with it to see if it actually works. Here she is putting some on a small spot on her left cheek. We shall see if it takes the spot away. So far the last couple of days it seems to be acting like a dermal peeling agent. The area gets dry and a layer of skin peels off.
|
Keto diet fights genetic Alzheimer’s
People with the APOE4 gene variant are highly likely to end up with Alzheimer’s. These folks, particularly women, metabolically have a hard time converting sugars (glucose) into energy for the brain. A keto diet avoids this problem by providing ketones as energy for the brain. This helps prevent degeneration of brain cells.
More
___________________________
“Principle of optimism. Focusing on and building more of what you like works better than focusing on trying to stop what is wrong.“~David DeLapp
_____________________________________
Green tea improves insulin sensitivity and muscle mass 
Daily consumption of green tea is found to improve insulin sensitivity, reduce weight, maintain muscle mass, and protect the body from the effects of a high fat diet. This study was done on mice and they used a very high dose of green tea extract to get these results. But cultures that normally drink green tea many times a day also show these benefits.
More
____________________________
“Principle of humility. Recognizing that your needs are the same as everyone else allows for balanced and even exchanges that are mutually beneficial.“
~David DeLapp
________________________________________
Social ties slow aging
Family ties, friendships, and community connections  have been shown to reduce inflammation, lower stress hormones, and slow down the cellular clock for aging. These benefits held strong regardless of income, education, living situation. have been shown to reduce inflammation, lower stress hormones, and slow down the cellular clock for aging. These benefits held strong regardless of income, education, living situation.
More
________________________
“Principle of willingness and surrender. You can not move if you first do not give up where you are. Willingness to surrender the parts of your identity story that are not working for you is the first step to change.“
~David DeLapp
|

